Interventional Care


We notice that you are visiting us from . This site only services US-based visitors. Would you like to visit the site that is appropriate for your location?

As of 11 January 2022, the U.S. had approximately 62 million cases of COVID-19 leading to 839,500 deaths. COVID-19 cases in the U.S. are now exceeding greater than 200,000 cases per day with the current level of cases exceeding those seen during the Delta-peak (Aug.-Sept. 2021)3. According to the New York Times on 11 January 2023, over the past 14 days, COVID-19 cases have increased by 203%, tests have increased by 34%, hospitalizations have increased by 83% and deaths have increased by 36%. According to the New York Times, the dramatic increase in COVID-19 cases worldwide and in the U.S. is being largely driven by the emergence of the Omicron variant of SARS-CoV-2.
On November 30, 2021, Omicron was designated by the U.S. Government as a variant of concern based on the following:
The risks of acquiring Omicron and developing the serious disease can be mitigated by precautionary measures (see below for full list). However, all persons should follow the guidance of the U.S. Centers for Disease Control and Prevention (CDC), and their state and local public health departments. CDC provides specific COVID-19 prevention guidance for many settings including healthcare facilities, workplaces, K-12 schools, colleges and universities, cruise ships, jails and prisons, and nursing homes. These recommendations will reduce (the transmission) but cannot eliminate the possibility of acquiring COVID-19.
COVID-19 vaccines are safe and effective. The CDC recommends that all persons 5 years or older should receive a full vaccine series. The Pfizer vaccine is available for persons 5 years and older, while the Moderna vaccine is available for persons 18 years and older. Booster doses provide substantially increased protection against SARS-CoV-2 infection and the development of serious disease, especially the Omicron variant. Therefore, it is recommended that all eligible persons 12 years of age and older receive a COVID-19 vaccine booster. A complete vaccine series provides better protection against Omicron than does prior infection, so all persons who have had COVID-19 should receive a complete vaccine series. Pregnant women are explicitly recommended to receive a COVID-19 vaccine by the CDC.
According to the CDC, masking provides substantial protection against acquiring COVID-19. Ideally, masks should be worn by all persons when indoors or outside of their home, regardless of whether the person has had COVID-19 or is vaccinated.
Omicron is highly infectious, and immunity from prior exposure or being fully vaccinated does NOT provide good protection against Omicron. Ideally, a medical mask should be used, however, multiple homemade masks are acceptable protection. The mask must cover the nose and mouth and should fit snuggly. Simple measures can improve the fit of the mask.1
When indoors or outside of one’s home, and when masking by all persons is not possible, physical distancing is crucial. It is recommended that a 6-foot distance separate all unmasked persons. However, a minimum of 3-feet should always be used.
SARS-CoV-2 can survive on hands for minutes to hours, but it is rapidly inactivated within 15 seconds by the use of a waterless alcohol product (i.e., 60 to 90% alcohol). NOTE: Soap and water are also effective. It is important that hand hygiene be practiced when outside one’s home after contact with any potentially contaminated products.
SARS-CoV-2 can survive on environmental surfaces for minutes to hours, sometimes days. Therefore, potentially contaminated surfaces should be disinfected with an EPA registered disinfectant on List-N. Cleaning with soap and water for surfaces outside of healthcare facilities instead of disinfection is recommended by the CDC.
Being in crowded places like restaurants, bars, fitness centers, or movie theaters puts you at higher risk for exposure to COVID-19. Where possible, avoid indoor spaces that do not offer fresh air from the outdoors. If indoors, consider opening windows and doors to let in fresh air, where possible.
The CDC provides specific recommendations for both U.S. and international travel. Persons planning to travel are highly recommended to review these recommendations. Persons traveling abroad should check with their airline and review the websites of their countries of destination, as well as any interim stops. However, provided individuals have been fully vaccinated and boosted prior to travel and remain masked during travel, the risk is not the travel per se, but what activities occur at the travel destination.
Persons who develop signs and/or symptoms of COVID-19 should immediately contact their healthcare provider AND stay home. Several available therapies reduce the risk of infected persons developing serious disease including hospitalizations and death. Therefore, early testing for COVID-19 and contacting a healthcare provider is crucial, especially for persons at risk for serious disease (e.g., older adults, very young children, persons with underlying diseases).
People with COVID-19 have had a wide range of symptoms reported – ranging from mild symptoms to severe illness. Symptoms may appear 2-14 days after exposure to the virus. Anyone can have mild to severe symptoms, including fever or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, and/or diarrhea. Be sure to look for emergency warning signs for COVID-19, including trouble breathing, persistent pain or pressure in the chest, new confusion, inability to wake or stay awake, or pale, gray, or blue-colored skin, lips, or nail beds, depending on skin tone. If someone is showing any of these signs, seek emergency medical care immediately. If you experience any other symptoms that are severe, please call your medical provider immediately. You can also call 911 or call ahead to your local emergency facility. Be sure to notify the operator that you are seeking care for someone who has or may have COVID-19.
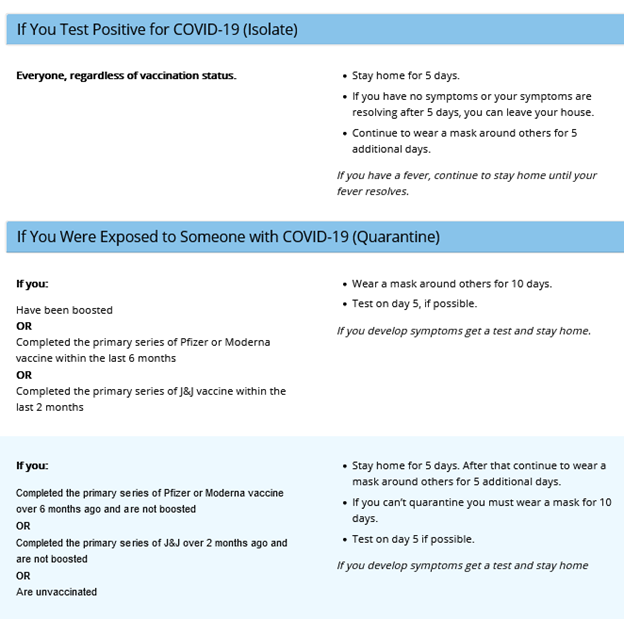
The CDC has recently updated their recommendations for isolation and quarantine for the general public after developing COVID-19 or being exposed, learn more by visiting their website here.
References: