Interventional Care


We notice that you are visiting us from . This site only services US-based visitors. Would you like to visit the site that is appropriate for your location?
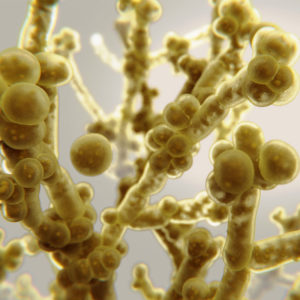
C. auris is an emerging fungal microorganism that is often resistant to antifungal disinfectants. Evidence shows that it can survive on health care environmental surfaces.
Studies have shown that auris can persist on surfaces in the health care environment for at least 14 days (Piedrahita et al., 2017; Welsh et al., 2017); C. auris has been cultured from contaminated bedding for up to 7 days (Biswal et al., 2017).
The EPA recently announced that products that make a claim against drug-resistant Candida auris must submit data using a specified test method and the Candida auris strain AR Bank #0385.5 Proper disinfection of environmental surfaces using disinfectants effective against C. auris is important to help prevent the spread of Candida auris.
PDI Healthcare offers several products that are effective against Candida auris:
In addition to surface disinfectants, UVC has been shown effective against C. auris as well.
According to a study, “Inactivation of Candida auris and Candida albicans by ultraviolet-C,” the Tru-D® device was shown effective against C. auris in both direct and indirect line of sight. In the study, the Tru-D device was set on the vegetative bacterial cycles varying from 17-19 minutes.
“Tru-D SmartUVC and PDI Healthcare believe in a layered approach to disinfection to include hand hygiene, antibiotic stewardship, thorough manual cleaning/disinfection and enhanced disinfection using UVC light energy,” Alice Brewer, MPH, CIC, CPHQ, FAPIC, for Tru-D SmartUVC, said. “A combination of PDI products together with the Tru-D technology can help provide the cleanest environments possible.”
References