Interventional Care


We notice that you are visiting us from . This site only services US-based visitors. Would you like to visit the site that is appropriate for your location?
Clostridioides difficile, formerly Clostridium difficile, (C. diff.) is a bacterial pathogen of significant notoriety amongst healthcare professionals. C. diff. infection is now the most common healthcare-associated infection (HAI) in the United States, with nearly a quarter of a million cases amongst hospitalized patients in 20171. The most severe of these cases, typically in patients over 65, can be deadly1,2.
C. diff. transmission between patients occurs through physical contact with a contaminated environment. As a result, an effective infection prevention and control strategy requires thorough cleaning and disinfection of the healthcare devices and facilities in contact with infected patients1,3.
Despite the need for an effective infection prevention and control strategy, C. diff. is significantly more difficult to disinfect compared to other HAI-causing bacteria. Surface disinfection of MRSA and pathogenic E. coli, for example, can be achieved by a variety of active chemical ingredients, including quaternary ammonium and alcohol. C. diff. however, is resistant to these foundational disinfectant chemistries4.
Why is C. diff. so difficult to disinfect?
The heightened resilience of C. diff. is due to its unique adaptations to survival outside the mammalian gastrointestinal tract. C. diff. infection is a gastrointestinal disease which causes symptoms ranging from mild diarrhea to severe pseudomembranous colitis (inflammation of the intestine)5. Here in the GI tract C. diff. thrives, producing the toxins responsible for the symptoms associated with infection6. However in order to survive outside the human body long enough to be transmitted to a new host, C. diff. undergoes a physical transformation into a spore before being released with feces.
Bacterial spores are specialized cellular structures adapted for surviving the potentially harsh physical and chemical stresses present in the environment7. This distinct physical structure, characterized by a unique cellular envelope architecture and dehydrated cellular core8, allows C. diff. to persist in the environment as well as resist inactivation by quaternary ammonium compounds and alcohol4,9.
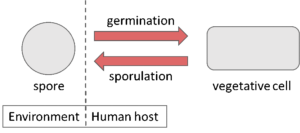
Fig. 1: Diagram of C. diff. life cycle.
Effective C. diff. sporicidal disinfectants
While C. diff. disinfection is relatively challenging, a few tools are at our disposal. Strong oxidizing chemicals are capable of inactivating bacterial spores such as sodium hypochlorite (bleach) and hydrogen peroxide10. As a result, these chemistries have been utilized to produce hospital-grade disinfectants with sporicidal efficacy, including PDI’s Sani-Cloth® Bleach Germicidal Wipes and Sani-HyPerCide™ Germicidal Spray respectively.
Additionally ‘no-touch’ UV-C devices have become attractive alternatives to chemical-based disinfection. While C. diff. spores are relatively resistant to UV-C when compared to other HAI-causing bacteria, increased reflected doses are capable of reducing C. diff. spores in healthcare settings11.
C.diff. infection impacts nearly a quarter of a million people every year. And the unique biology of this bacterial pathogen makes infection prevention and control particularly challenging. However with an understanding of how and why C. diff. presents these challenges, we can be better prepared to combat this important HAI.