Interventional Care


We notice that you are visiting us from . This site only services US-based visitors. Would you like to visit the site that is appropriate for your location?

As part of a public health containment response, on July 26th 2019, the CDC updated their guidance for LTC settings and the use of PPE to include a new level of precautions called Enhanced Precautions1. The goal of Enhanced Precautions was to inhibit the ongoing problem of the silent spread and colonization of MDRO’s in the LTC setting by using a level of precautions above standard, but below transmission. However, with the arrival of the new novel coronavirus in early 2020, more confusion has arisen now that even further specifics around COVID-19 is expected.
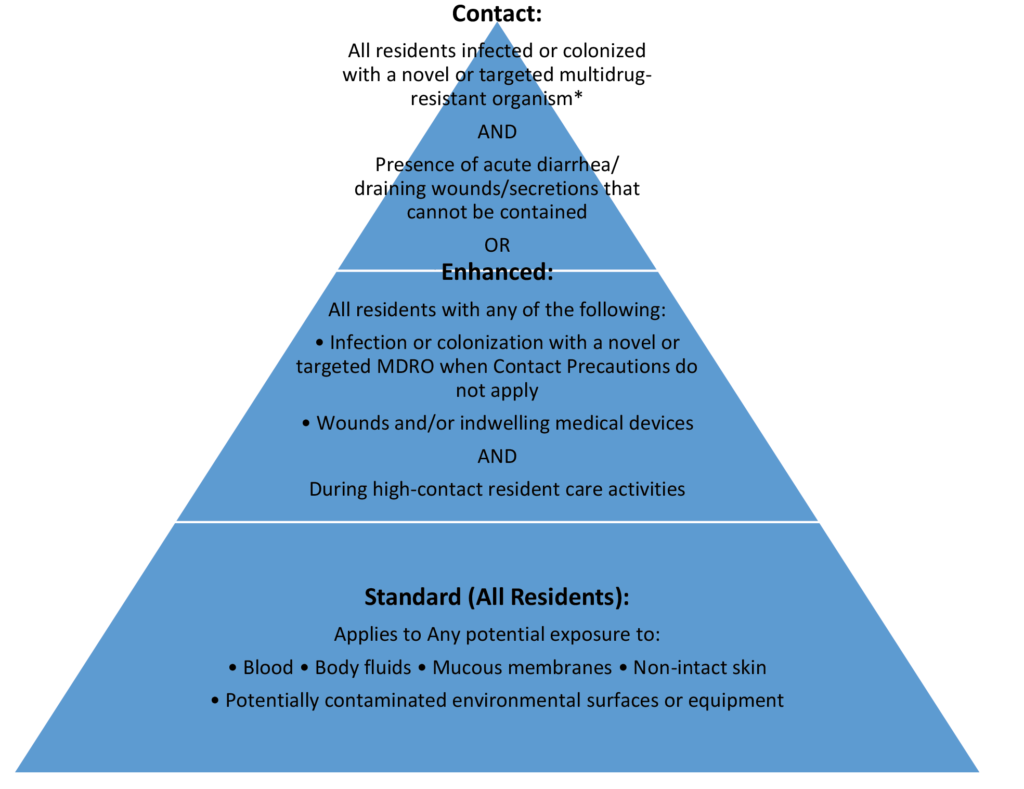
Let’s look at the different levels of precautions and try to clarify when each is supposed to be used and why1.
Standard Precautions:
Standard Precautions is the most basic of precautions and evolved from the original term of Universal Precautions. It is considered a standard of care that all healthcare professionals must follow. It assumes that all residents, regardless of diagnosis or status, have potentially infectious blood and bodily fluids. Healthcare workers must wear personal protective equipment appropriate for the task being performed, such as gloves, gown, mask and face shield for activities that may generate splashes or aerosols, to just wearing gloves for more basic activities. Washing hands before and after contact with the resident and the residents’ surroundings is emphasized as a key component, as well as safe injection practices, respiratory hygiene and cough etiquette, environmental cleaning and disinfection, and reprocessing of reusable medical equipment.1
Contact Precautions:
Contact Precautions are the only “next level” precautions really required in long term care. It is considered to be transmission based. There are three levels of transmission based precautions; contact, droplet, and airborne (although airborne is rarely if ever used in LTC settings).
The goal of Contact Precautions is to interrupt the spread of MDRO’s from direct or indirect contact with the resident or the resident’s environment. Residents infected or colonized with a novel or targeted multidrug-resistant organism with presence of acute diarrhea, draining wounds or other sites of secretions or excretions that are unable to be covered or contained are placed in Contact Precautions1. This level of precautions requires that healthcare personnel wear a gown and gloves (plus face mask/eye shield, for droplet precautions) prior to crossing the door threshold for EVERY ENTRY into a resident room regardless of the type of care being given.. It also may include the use of dedicated equipment, private rooms or cohorting, and restriction to the room of the infected or colonized resident. Because of the more stringent nature of this level of precautions, they are intended to be time limited.
Enhanced Precautions:
July 2019 saw the arrival of a new level of precautions from the CDC for LTC facilities. Enhanced Precautions recognizes that there may be a silent spread of organisms of concern (these are defined as pan-resistant organisms, Candida auris and carbapenemase-producing organisms (., Pseudomonas spp and Acinetobacter baumannii)3 occurring from residents that may not be identified as colonized or infected during high-risk activities that often spread organisms to the environment, or to the hands and clothing of health care workers.4,5 These activities include: bathing, toileting, device care, and wound care. The expectations for Enhanced Precautions are that the healthcare worker wear gloves and a gown for all such activities, regardless of diagnosis or infection status. The goal is to stop the ongoing silent spread and transmission of organisms from unknown sources. This level of precautions does NOT require resident restriction to rooms, or strict gowning and gloving upon entry to the room every time, but rather just during high-risk activities. Also, there is no time limit to this level of precautions. Enhanced Precautions differs from Standard Precautions in that Standard Precautions requires PPE based on anticipated exposure, whereas Enhanced Precautions assumes exposure will occur with certain activities and preemptively requires a set type of PPE during those tasks.
COVID-19 Precautions:
With the unexpected arrival of the novel coronavirus, there are even more expectations. Initially, there were almost daily updates to the expectations of what the CDC wanted long term care facilities to do around personal protective gear. Now, the CDC has a dedicated website page specifically for COVID-19 prevention and LTC facilities which includes the expectations of PPE. Precautions if COVID-19 is identified in the facility is that all residents should be restricted to their rooms, no visitors are allowed, and healthcare personnel should wear an N-95 or higher level respirator (or face mask if unavailable), eye protection, gloves and a gown2. This approach is recommended because of the high-risk of unrecognized infection among residents. Recent finding suggests that a substantial proportion of residents could have COVID-19 without reporting symptoms or before symptoms develop.
Conclusion:
The determination of precaution type is left largely up to the facility based on diagnosis and facility risk assessment. The length of time a resident must remain in contact precautions is also left up to the facility, and based on the level of risk transmission the resident and their diagnosis poses along with the evidence of ongoing transmission within that unit or ward. Although PPE requirements can seem daunting, the main thrust of a PPE program within LTC should be to stop the spread of any organism from one resident to the next through the environment or the clothing and hands of healthcare workers with the use of personal protective gear.
Looking for more support around this topic? Take our “Coronavirus Prevention in Long-Term Care Settings” FREE Continuing Education Course!